THREE years ago, on January 13th, Rukhsar Khatun, then 15 months old,
was diagnosed with polio. She now has a crippled leg and struggles to
keep up with her friends. But this little girl, from a West Bengali
village, can claim some fame: she is, with luck, the last Indian to be
infected with the wild polio virus. Enough time has passed with no new
case for India shortly to be certified as free of the scourge.
That is a big success. India’s anti-polio campaign began in 1995 with
severe disadvantages. The country spends little on public health,
barely 1% of GDP, and has been awful at immunising children. Too few
parents know the basics of hygiene and nutrition, let alone the benefits
of vaccines. India has bad sanitation, large remote populations and
vast migration from village to slum.
Yet much has gone right. The anti-polio campaign received over $3
billion, mostly from within India itself, and deployed 2.4m vaccinators.
Unicef, the World Health Organisation (WHO), Rotary International and
the Gates Foundation (both charities) gave technical help. Religious
leaders reassured people suspicious about vaccinations, and politicians
knocked on doors to make sure children took their medicine.
At the peak of coverage, 99.7% of the target population swallowed
anti-polio drops, says Anuradha Gupta of the national health ministry.
That is startlingly high, considering that a decade ago “universal”
vaccination coverage for seven preventable diseases (such as diphtheria,
tetanus, hepatitis B) was a pitiful 30% in Bihar, a big, poor northern
state.
India’s campaign has been successful enough for its lessons to be
applied in Pakistan, Afghanistan and Nigeria, the last places with
endemic polio (foreign fighters may have reintroduced it to Syria, too).
Vaccinators learned to attend especially to mobile populations, like
seasonal workers at brick kilns, and found that many migrants are best
reached not at home but in bus and railway stations.
Good monitoring was crucial, too. In Uttar Pradesh and Bihar,
vaccinators visited 60m households several times a year, says Hamid
Jafari of the WHO. To compile data on recipients, some 400,000
hard-to-reach population groups were carefully tracked and plotted, down
to each household. Data passed early to decision-makers, at the
district-official level, allowed a quick response to new cases.
India now looks more capable of fighting other, deadlier, diseases.
It plans to eradicate measles by 2020. That killed 66,000 children a
year as recently as 2010, half the world total that year. In the past
three years 140m children have been injected with extra doses of measles
vaccine, so the toll should have fallen. Universal vaccination coverage
is rising, too. In Bihar it has reached 70%. Ms Gupta suggests that
nationally it is above 78%.
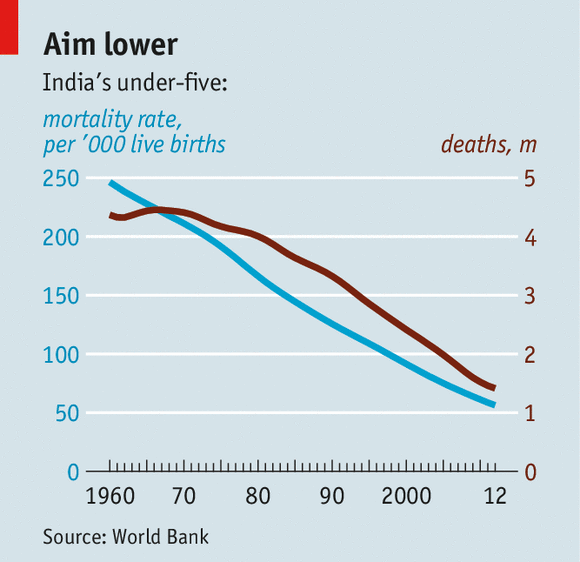
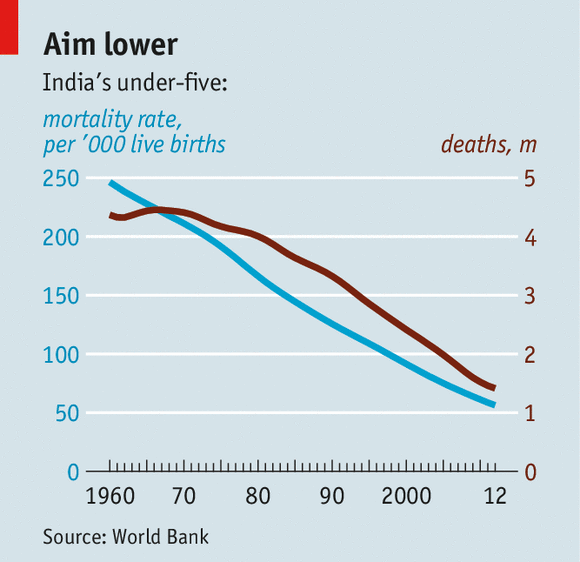
The next step is to give the army of vaccinators more tasks. A
vaccine is being developed against diarrhoea—responsible for the deaths
of many of the 1.4m Indian infants and toddlers who still die every year
(see chart). The vaccinators could also lead a planned campaign on
hygiene and nutrition. A screening programme, launched in 2012, involves
5,000 mobile health centres. These have diagnosed 700,000 children with
one of 30 common medical conditions and treated, so far, 100,000 of
them. Spreading education, as well as care, would bring greater success
yet.
"The next step is to give the army of vaccinators more tasks.
also it is important to not slack on required vaccinations .
I keep seeing news about diphtheria /measles /tetanus /taking children's lives all over India sporadically."