Breast Cancer
In this module, you will be introduced to some basic information about breast cancer: statistics related to breast cancer, types of breast cancer, risk factors, anatomy of the breast, abstracting, coding, staging and treatment of breast cancer.
Introduction to Breast Cancer
Breast cancer is a malignant cell growth in the breast. If left untreated, the cancer spreads to other areas of the body. Excluding skin cancer, breast cancer is the most common type of cancer in women in the United States, accounting for one of every three cancer diagnoses.
An estimated 211,240 new invasive cases of breast cancer were expected to occur among women in the United States during 2005. About 1,690 new male cases of breast cancer were expected in 2005.
The incidence of breast cancer rises after age 40. The highest incidence (approximately 80% of invasive cases) occurs in women over age 50.
In addition to invasive breast cancer, 58,590 new cases of in situ breast cancer are expected to occur among women during 2005. Of these, approximately 88% will be classified as ductal carcinoma in situ (DCIS). The detection of DCIS cases is a direct result of the increased use of mammography screening. This screening method is also responsible for detection of invasive cancers at a less advanced stage than might have occurred otherwise.
An estimated 40,870 deaths (40,410 women, 460 men) were anticipated from breast cancer in 2005. Breast cancer ranks second among cancer deaths in women. According to the most recent data, mortality rates declined significantly during 1992-1998, with the largest decreases in younger women, both white and black.
Types of Breast Cancer
Ninety percent of breast cancer are adenocarcinomas, which arise from glandular tissue. Within this broad category, there is a great degree of variation. For instance, there are about 30 different subtypes of adenocarcinoma.
The earliest form of the disease, ductal carcinoma in situ, comprises about 15-20% of all breast cancers and develops solely in the milk ducts. The most common type of breast cancer, invasive ductal carcinoma, develops from ductal carcinoma in situ, spreads through the duct walls, and invades the breast tissue.
Cancer that begins in the lobes or lobules is called lobular (small cell) carcinoma and is more likely to be found in both breasts. Invasive lobular carcinoma originates in the milk glands and accounts for 10-15% of invasive breast cancers. Both ductal and lobular carcinomas can be either in situ, or self-contained; or infiltrating, meaning penetrating the wall of the duct or lobe and spreading to adjacent tissue.
Less common types of breast cancer include the following:
- Inflammatory breast cancer (diffuse brawny infiltration; breast appears red or inflamed; tends to spread quickly)
- Medullary carcinoma (originates in central breast tissue)
- Mucinous carcinoma (invasive; usually occurs in postmenopausal women)
- Paget disease of the nipple (originates in the milk ducts and spreads to the skin of the nipples or areola)
- Phyllodes tumor (tumor with a leaf-like appearance that extends into the ducts; rarely metastasizes)
- Tubular carcinoma (small tumor that is often undetectable by palpation)
Sarcomas (cancer of the connective tissue) and lymphomas (cancer of the lymph tissue) rarely develop in the breasts.
Risk Factors
The risk factors of breast cancer are unknown, although studies suggest that estrogen, the female hormone produced by the ovaries, is involved. One reason for suspecting estrogen is the association of breast cancer to certain reproductive system changes in a woman's life.
About 5% -10 % (per ACS literature) of all breast cancers are thought to be related to genetic predisposition. Molecular tests are available to identify BRCA1 and BRCA2 genetic susceptibility, which is present in a small percentage of the population. BRCA1 and BRCA2 mutations are seen more often in women of Jewish ancestry.
It has already been established that women with first-degree relatives who had breast cancer are at greater risk of getting it themselves. These women are encouraged to have screening tests earlier and sometimes more often than women without such a family history.
The risk of breast cancer increases with age. The lifetime risk is approximately 1 in 8. The risk increases significantly after age 50 with the risk for 50-year-olds at 1 in 37; 60-year-olds 1 in 26 and for 70-year-olds 1 in 24. Risk is higher in women who have a personal or family history of breast cancer, biopsy-confirmed atypical hyperplasia, increased breast density, a long menstrual history (menstrual periods that started early and ended late in life), obesity after menopause, recent use of oral contraceptives or postmenopausal estrogens and progestin, who have never had children or had their first child after age 30, or who consume alcoholic beverages.
Worldwide, breast cancer incidence rates appear to correlate with variations in diet, especially fat intake, although the specific dietary factors that affect breast cancer have not been firmly established. Vigorous physical activity and maintenance of a healthy body weight are associated with lower risk. Most data indicate tamoxifen decreases breast cancer risk and preliminary data suggest another selective estrogen-receptor modulator, raloxifene, does also.
Signs & Symptoms
The earliest sign of breast cancer is an abnormality that shows up on a mammogram before it can be felt by the woman or her health care provider. When breast cancer has grown to the point where physical signs and symptoms exist, a breast lump, or tenderness; skin irritation or dimpling; and nipple discharge and/or pain, scaliness, ulceration, or retraction may be noticed. Breast pain is commonly due to benign conditions and is not usually the first symptom of breast cancer.
Mammography is especially valuable as an early detection tool because it can identify breast cancer at an early stage before physical symptoms develop. Studies have shown that early detection saves lives and increases treatment options. The reduction in breast cancer mortality have been attributed, in large part, to the regular use of screening mammography and awareness education. The American Cancer Society recommends that women age 40 and older have an annual mammogram, an annual clinical breast examination by a health care professional (close to and preferably before the scheduled mammogram), and perform monthly breast self-examination. Women ages 20-39 should have a clinical breast examination by a health care professional every three years and should perform breast self-examination monthly.
When a woman has a suspicious lump or other abnormality on an initial mammogram, further testing can help determine whether additional tests are needed. Mammography alone does not provide a sufficient assessment. All suspicious lumps should be biopsied for a definitive diagnosis.
Five-Year Survival Rates
| Years | Survival Rate |
|---|---|
| 5yr | 88% |
| 10yr | 80% |
| 15yr | 71% |
| 20yr | 63% |
| Stage | Survival Rate |
|---|---|
| State 0 | 100% |
| State I | 98% |
| State IIA | 88% |
| State IIB | 76% |
| State IIIA | 56% |
| State IIIB | 49% |
| State IV | 16% |
| Stage | Survival Rate |
|---|---|
| Stage 0 | 93% |
| Stage I | 88% |
| Stage II | 77% |
| Stage III | 51% |
| Stage 4 | 16% |
| Overall | 78% |
Review: Introduction to Breast Cancer
Here is what we have learned from Introduction to Breast Cancer:
- Breast cancer is malignant cell growth in the breast. If left untreated, the cancer can spread to other areas of the body.
- Breast cancer is the second most common type of cancer in women and the second leading cause of cancer-related death in women.
- The causes of breast cancer are unknown; however, studies suggest that the growth of breast cancer is often affected by the presence of estrogen.
- The earliest sign of breast cancer is an abnormality that shows up on a mammogram before it can be felt by the woman or her health care provider.
- Most breast cancer develops in glandular tissue and is classified as adenocarcinoma; less common types of breast cancer include inflammatory breast cancer, medullary carcinoma, mucinous carcinoma, Paget disease of the nipple, phyllodes tumor, and tubular carcinoma.
Breast Anatomy
The breasts of an adult woman are milk-producing, tear-shaped glands. They are supported by and attached to the front of the chest wall on either side of the breast bone or sternum by ligaments. They rest on the major chest muscle, the pectoralis major.
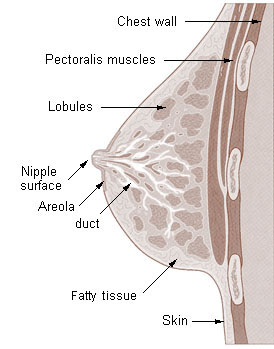
The breast has no muscle tissue. A layer of fat surrounds the glands and extends throughout the breast.
The breast is responsive to a complex interplay of hormones that cause the tissue to develop, enlarge and produce milk. The three major hormones affecting the breast are estrogen, progesterone and prolactin, which cause glandular tissue in the breast and the uterus to change during the menstrual cycle.
Each breast contains 15 to 20 lobes arranged in a circular fashion. The fat (subcutaneous adipose tissue) that covers the lobes gives the breast its size and shape. Each lobe is comprised of many lobules, at the end of which are tiny bulb like glands, or sacs, where milk is produced in response to hormonal signals.
Ducts connect the lobes, lobules, and glands in nursing mothers. These ducts deliver milk to openings in the nipple. The areola is the darker-pigmented area around the nipple.
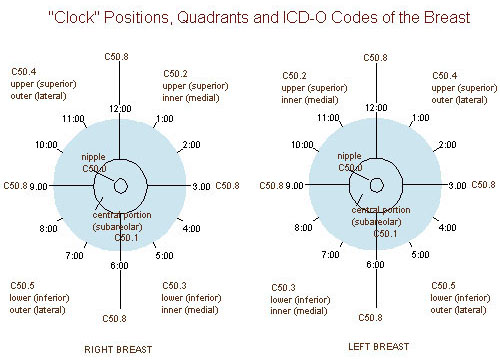
Quadrants of the Breast
Regional Lymph Nodes
Blood and lymph vessels form a network throughout each breast. Breast tissue is drained by lymphatic vessels that lead to axillary nodes (which lie in the axilla) and internal mammary nodes (which lie along each side of the breast bone). When breast cancer spreads, it is frequently to these nodes.

- Axillary lymphatic plexus
- Cubital lymph nodes *
- Superficial axillary (low axillary)
- Deep axillary lymph nodes
- Brachial axillary lymph nodes
- Interpectoral axillary lymph nodes (Rotter nodes)
- Paramammary or intramammary lymph nodes
- Parasternal lymph nodes (internal mammary nodes)
*Note: the cubital lymph nodes are not part of the lymph node drainage of the breast.
Read more about sentinel nodes.
Review: Breast Anatomy
Here is what we have learned from Breast Anatomy:
- The breasts of an adult woman are milk-producing, tear-shaped glands.
- A layer of fatty tissue surrounds the breast glands and extends throughout the breast, which gives the breast a soft consistency and gentle, flowing contour.
- The breast is responsive to a complex interplay of hormones that cause the breast tissue to develop, enlarge and produce milk.
- Each breast contains 15 to 20 lobes arranged in a circular fashion.
- Each lobe is comprised of many lobules, at the end of which are tiny bulblike glands, or sacs, where milk is produced in response to hormonal signals.
- Ducts connect the lobes, lobules, and glands; in nursing mothers, these ducts deliver milk to openings in the nipple.
- Breast tissue is drained by lymphatic vessels that lead to axillary nodes (which lie in the axilla) and internal mammary nodes (which lie along each side of the sternum).
ICD-O-3 Site Codes
In the second and third editions of ICD-O, cancers of the male breast are coded using the schema for tumors of the female breast.
| ICD-O-3 | Term | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C50.0 | Nipple | ||||||||||||
| C50.1 | Central portion of breast | ||||||||||||
| C50.2 | Upper-inner quadrant of breast (UIQ) | ||||||||||||
| C50.3 | Lower-inner quadrant of breast (LIQ) | ||||||||||||
| C50.4 | Upper-outer quadrant of breast (UOQ) | ||||||||||||
| C50.5 | Lower-outer quadrant of breast (LOQ) | ||||||||||||
| C50.6 | Axillary tail of breast | ||||||||||||
| C50.8 | Overlapping lesion of breast | ||||||||||||
| C50.9 | Breast, NOS (excludes Skin of breast C44.5); multi-focal neoplasm in more than one quadrant of the breast.Morphology & GradeICD-O-3 Morphology Codes
For diagnostic terms in the pathology report which are not part of the following list, refer to your ICD-O-3 manual.
Adenocarcinoma (ICD-O-3 code 81403)
Common combination morphologies
Behavior types
Synonyms for carcinoma in situ: noninfiltrating, intraductal, lobular carcinoma in situ, Stage 0, noninvasive, no stromal involvement, papillary intraductal, papillary non infiltrating, intracystic, lobular neoplasia, lobular noninfiltrating, confined to epithelium, intraepithelial, intraepidermal
Other morphologic terms: Paget disease (854_3)—crusty tumor of nipple and areola, which may be associated with underlying tumor of the ducts.
Inflammatory carcinoma (85303)—frequently involves entire breast and is characterized by reddened skin and edema caused by tumor spread to lymphatic channels of skin of breast, usually without an underlying palpable mass. Inflammatory carcinoma is a clinical diagnosis verified by biopsy of the tumor and overlying skin. Key words: lymphatic involvement of skin, peau d'orange, orange-peel skin, en cuirasse
Cystosarcoma phyllodes (90203)—a variant of mammary fibroadenoma; locally aggressive; rarely metastasizes
Bloom-Richardson grading system—Synonyms: Modified Bloom-Richardson (BR), Scarff-Bloom-Richardson (SBR), SBR Grading, BR Grading, Elston-Ellis modification of Bloom-Richardson grading system. The Bloom-Richardson grading scheme is a semi-quantitative grading method based on three morphologic features of invasive (no-special-type) breast cancers. The morphologic features are:
Seven possible scores are condensed into three BR grades. The three grades then translate into well-differentiated (BR low grade), moderately differentiated (BR intermediate grade) and poorly differentiated (BR high grade).
|
Extent of Disease Evaluation
Common Metastatic Sites
| Spread | Primary Site/Mets |
|---|---|
| Lymphatic Spread | Distant lymph nodes (supraclavicular, cervical, contralateral internal mammary, occasionally contralateral axillary) |
| Hematogenous Spread | Bone, liver, brain |
Definitions
Key words/possible involvement:
Terms which indicate possible involvement by tumor. Common terms are provided, but the list is not all-inclusive.
Other words/no involvement:
Other terms seen in reports which indicate an abnormality but do not indicate a neoplastic process. Common terms are provided, but the list is not all-inclusive.
Key Information
Information to look for in the report of the study. Key information helps define the extent of disease.
Diagnostic Studies
- Physical Exam
- Imaging
- Tumor Markers
- Endoscopies
- Pathology
Physical Exam
Key Information
Clinical size and location of tumor or masses; skin changes (inflammation, ulceration, dimpling, satellite nodules, erythema [redness]), fixation of tumor, involvement of opposite breast, discharge, palpable axillary nodes ("shotty" nodes, fixed or matted nodes), involvement of supraclavicular or cervical nodes.Go to the Physical Exam page of the Diagnostic Tests for more information
Imaging
Key Information
Size and location of primary tumor, involvement of distant sites.
- Mammogram
Unilateral (single breast), bilateral (both breasts), contralateral (side not suspected of containing cancer).Key words/possible involvement:
Lesion, mass, irregular density, clustered calcification, spiculation, mammary duct distortion or asymmetry, nodular density, skin or nipple thickening, enlarged lymph nodes.Key words/no involvement:
If there is no specific reference to visible abnormality in the breast under suspicion. - Chest X-Ray
- Imaging, Bone
- Imaging, Brain
- Imaging, Liver/spleen
For more information about imaging, you may visit the following pages in the Diagnostic Tests module: Other Imaging.
Tumor Markers
Key Information
Estrogen Receptor Assay (ERA)
A laboratory test of breast cancer tissue to determine the responsiveness of the tumor to hormone manipulation, endocrine therapy or removal of the ovaries. About 55% of ER positive tumors will respond to endocrine therapy. Tumors which are negative for estrogen receptors rarely respond to hormone manipulation. The unit of measurement is femtomoles (fmoles) per milligram of tumor.
Types of ERA:
Quantified (measured in femtomoles or fmoles)
Immunohistochemical
A qualitative measurement of the observed number of hormone responsive cells, reported as positive or negative.
Immunohistochemical
A qualitative measurement of the observed number of hormone responsive cells, reported as positive or negative.
Test results
Negative: 3 fmoles or less. ERA may not be performed if tumor is less than 1.0 cm in size or if the tumor is in situ.
Negative: 3 fmoles or less. ERA may not be performed if tumor is less than 1.0 cm in size or if the tumor is in situ.
Progesterone Receptor Assay (PRA)
A laboratory test of breast cancer tissue to determine the responsiveness of the tumor to endocrine therapy or to removal of the ovaries. Progesterone receptor assay increases the reliability of estrogen receptor assay results: a positive progesterone receptor assay indicates greater likelihood that the patient will respond to hormone therapy. The unit of measurement is femtomoles (fmoles) per milligram of tumor.
Types of PRA:
Quantified (measured in femtomoles or fmoles)
Immunohistochemical
A qualitative measurement of the observed number of hormone responsive cells, reported as positive or negative.
Immunohistochemical
A qualitative measurement of the observed number of hormone responsive cells, reported as positive or negative.
Test results
Negative: 5 fmoles or less. Test may not be performed if tumor is less than 1.0 cm in size or if tumor is completely in situ.
Negative: 5 fmoles or less. Test may not be performed if tumor is less than 1.0 cm in size or if tumor is completely in situ.
DNA Studies (also called flow cytometery)
A means of measuring certain physical and chemical characteristics of cells or particles as they travel in suspension one by one past a sensing point.
A means of measuring certain physical and chemical characteristics of cells or particles as they travel in suspension one by one past a sensing point.
Ploidy analysis
Aneuploid tumors correlate with more aggressive tumors and a greater risk of recurrence.
Aneuploid tumors correlate with more aggressive tumors and a greater risk of recurrence.
S-Phase (also called Cell Cycle Analysis)
Percentage of tumor cells synthesizing DNA; patients with high S-phase fraction have less favorable prognosis.
Percentage of tumor cells synthesizing DNA; patients with high S-phase fraction have less favorable prognosis.
Other Breast Cancer Tumor Markers
C219
Presence is associated with multidrug resistance.
Presence is associated with multidrug resistance.
Cathepsin D
Distinguishes node-negative patients who may recur (and therefore should receive adjuvant chemotherapy) from node-negative patients who probably will not recur. Elevation indicates a poorer prognosis.
Distinguishes node-negative patients who may recur (and therefore should receive adjuvant chemotherapy) from node-negative patients who probably will not recur. Elevation indicates a poorer prognosis.
CEA (Carcinoembryonic Antigen)
Persistent elevated levels indicate residual or recurrent metastatic carcinoma.
Persistent elevated levels indicate residual or recurrent metastatic carcinoma.
C-erb B-2 (also called HER-2 or neu oncoprotein)
Associated with larger sized tumors, shorter relapse time and lower survival rate.
Associated with larger sized tumors, shorter relapse time and lower survival rate.
C-myc DNA amplification
Elevated (amplified) in breast cancers in older women.
Elevated (amplified) in breast cancers in older women.
EGFR Epidermal Growth Factor Receptor)
Negative EGFR results correlate with better prognosis regardless of ER status.
Negative EGFR results correlate with better prognosis regardless of ER status.
Int-2 DNA Amplification
Elevation (amplification) associated with recurrence of tumor.
Elevation (amplification) associated with recurrence of tumor.
Go to the Tumor Markers page of the Diagnostic Tests module for more information.
Endoscopies
Not usually done for breast cancer; however, there are some studies done using endoscopy.
Go to the Endoscopies page of the Diagnostic Tests module for more information.
Pathology
Key Information
Cell type, exact size of malignment lesion, presence of multiple tumors in breast, size and number of lymph nodes involved (including micrometastases), extension to adjacent tissues (muscle, fascia, skin).
Cytology reports
Sentinel lymph node biopsy
Selective removal of one or more axillary lymph nodes identified by placing dye or a radioactive agent in the tumor bed and following the flow of the dye to specific lymph nodes. The lymph nodes which trap the dye or radioactivity are the first nodes in the lymphatic drainage of the tumor and as such are more likely to contain metastases if present. If the sentinel lymph nodes are negative, there is a 95% chance that all other axillary lymph nodes are negative also.
Staging
Criteria for TNM Clinical Staging:
Physical examination; palpation of breast, axillary, supraclavicular and cervical nodes; pathologic examination of breast or other tissue to establish a diagnosis of cancer, including size of tumor, chest wall invasion, and presence or absence of positive nodes and distant metastases.
Criteria for TNM Pathologic Staging:
Removal of all primary tumor (no tumor at any margin of resection on gross examination) and at least Level I nodes (lateral to lateral border of pectoralis minor—at least 6 nodes in this area).
| Tis | In situ |
|---|---|
| T1 | 2cm |
| T1mic | 0.1 cm |
| T1a | > 0.1 to 0.5 cm |
| T1b | > 0.5 to 1 cm |
| T1c | >1 to 2 cm |
| T2 | >2 to 5 cm |
| T3 | > 5 cm |
| T4 | Chest wall/skin |
| T4a | Chest wall |
| T4b | Skin edema/ulceration, satellite skin nodules |
| T4c | Both 4a and 4b |
| T4d | Inflammatory carcinoma |
| N1 | Movable axillary pN1 |
| N2 | Fixed axillary |
| N3 | Internal mammary |
| pN1a | Micrometastases only, # 0.2 cm |
| pN1b | Gross metastases i 1-3 nodes, >0.2 to < 2 cm ii 4 nodes/>0.2 to < 2 cm iii through capsule/ < 2 cm iv 2 cm |
Collaborative Stage Elements
For more details on Collaborative Stage, see the Intro to Collaborative Staging module.
Abstracting Keys
Tumor size is the primary differential in TNM staging. Use the size of tumor reported on the pathology report for best information. Measure the size of the invasive component to assign T category.
If the size is given by physical examination only, use major TNM T-category headings only (T1, T2, etc .) If size is provided by mammography or pathology report, use subcategories T1a, T1b, etc.
Use TX if the primary tumor was excised at another facility and no information about tumor size is available.
If tumor was found by mammography, or if there is no palpable tumor in the breast, indicate that this is the case.
Do not add together the sizes of pieces of tumor removed at biopsy and at resection. Use the largest size of tumor, even if this is from the biopsy specimen. If no size is stated, record as 999 in the field "Size of Tumor".
If a specific size is not given, record size of tumor as 998 if involvement of breast is described as diffuse or inflammatory carcinoma.
Multifocal tumors in the same breast that are grossly measureable should be staged according to the size of the largest tumor.
Tumors of different histologies should be considered separate primaries if the difference is at the level of the 3-digit ICD-O morphology code.
If ductal and lobular neoplasms are diagnosed concurrently in different quadrants of the same breast, the ICD-O site code should be C50.9.
Simultaneous bilateral tumors should be staged separately. Simultaneous is defined as being diagnosed within two months.
Clusters or clumps of cancer cells found in axillary fat that are not specifically identified as lymph nodes are considered to be axillary lymph nodes that have lost their architectural configuration.
If a wedge resection of the breast is performed done for diagnosis and a more complete procedure, such as a modified radical mastectomy, is done as cancer-directed surgery, code the more complete surgical procedure. The
surgical code should indicate the status of the primary organ at the completion of the procedure.
surgical code should indicate the status of the primary organ at the completion of the procedure.
Surgery is the most common treatment for breast cancer. If no surgery was performed, indicate the reason in the "Reason for No Surgery" field.
Skin dimpling and nipple retraction do not alter the staging of the tumor, but should be noted. They are caused by tension on Cooper's ligament within the breast.
Adherence, attachment, fixation, induration and thickening are considered clinical evidence of extension to skin or subcutaneous tissue of breast.
Skin edema, peau d'orange, encuirasse, inflammation, skin ulceration indicate extensive skin involvement.
Fixation to pectoral fascia (the covering of the muscle) does not influence stage.
Paget's disease of nipple without an underlying tumor in the breast is staged as "Tis" disease. Paget's with other disease is measured by the size of the underlying tumor.
Breast Cancer Treatment
Treatment of breast cancer is among the most widely studied of all cancer therapies. New approaches to therapy and refinements in accepted regimens are constantly being evaluated and may rapidly become part of standard treatment protocols. Geographic practices also influence what is considered standard. Users should continually update their knowledge of cutting edge and standard treatment patterns.
Local control of the cancer occur more often when the tumor is small and can be completely removed by surgery. In the most advanced stages, breast cancer treatment begins with excision of the tumor or destruction of the tumor by radiation therapy. Surgery is frequently accompanied by some type of adjuvant treatment—radiotherapy, chemotherapy, hormonal therapy, immunotherapy, and other therapies.
Below is the information about treatment options by stage. The following sections will provide you with more detailed discussions about different therapies for breast cancer treatment.
Treatment Options by Stage
Intraductal Carcinoma
Total mastectomy; excisional biopsy with radiation therapy
Lobular Carcinoma in situ
Stage I (negative nodes)
Excisional biopsy/lumpectomy or segmental/wedge/partial breast resection with separate axillary node dissection and radiation to breast; modified radical or total mastectomy with axillary dissection. Adjuvant chemotherapy for estrogen receptor negative patients; adjuvant tamoxifen for estrogen receptor positive patients.
Stage II
Excisional biopsy/lumpectomy or segmental/wedge/partial breast resection with separate axillary node dissection and radiation to breast; modified radical or total mastectomy with axillary dissection; radical mastecomy (if needed to accomplish complete resection of tumor). Adjuvant chemotherapy (CMF, CAF, CA+/-tamoxifen, L-PAM + 5-FU, L-PAM, 5-FU + tamoxifen, PAF, CMFVP, tamoxifen alone)
Stage IIIA (operable)
Modified radical mastectomy or radical mastectomy with either radiation or chemotherapy. Radiation could be preoperative external beam radiation or postoperative external beam radiation with a booster dose to primary site. Chemotherapy could be CMF, CA, CAF, CMFP, CMFVP, L-PAM and 5-FU with or without tamoxifen
Stage IIIB (inoperable, including inflammatory)
Incisional biopsy plus external beam radiation to primary and regional nodes, followed by boost to local area plus interstitial implants to primary. Mastectomy thereafter if technically feasible, followed by chemotherapy or endocrine manipulation. Chemotherapy could be CMF, CAF, CMFP, CA, CMFVP. Endocrine therapy could include oophorectomy, tamoxifen, progesterone or androgens.
Stage IV
Biopsy followed by external beam radiotherapy to primary or mastectomy to control local disease. Hormonal therapy if estrogen receptor positive (oophorectomy, tamoxifen or progestational agent). Chemotherapy (CMF, CAF, CMFP, CMFVP, CA)
Surgery
In the past, a positive biopsy was followed immediately by surgical treatment. This was called a one-step process. Currently, when a biopsy confirms that a tumor is malignant, the decision about treatment is deferred for a week or more to allow the patient and family to explore treatment options with the patient's doctor.
Separating the diagnostic test from the surgery is called a two-step process. Although it requires another visit to a hospital and a second procedure, a two-step process allows a woman and her doctor to discuss and contemplate treatment options. Moreover, there is time to seek a second opinion. More definitive laboratory analysis of the biopsied tissue can be done during this time. In some cases, when the tumor is very small, it may be completely removed by the biopsy and additional surgery may not be necessary.
When planning therapy, an oncologist and/or surgeon considers the following factors: the stage of the cancer (that is, the size of the tumor, whether or not the lymph nodes are involved, and the presence of metastases); the tumor's hormone status; the woman's age and menopausal status; and her general health, including whether she has any serious and/or chronic illness or conditions, such as heart disease, that might be complicated by treatment. In some cases, doctors will want to consider other prognostic factors that indicate the tumor's aggressiveness and likelihood of recurrence. Treatment choices may be affected by ominous pathological features such as necrosis or comedeocarincoma or high grade.
Types of breast cancer surgery include lumpectomy, partial (or segmental) mastectomy, total (or simple) mastectomy, modified radical mastectomy, and radical mastectomy.
Lumpectomy and partial mastectomy are breast conserving surgeries. In lumpectomy, the cancerous lump and a margin of normal tissue around it are removed. Depending on the size and location of the cancer, partial (or segmental) mastectomy can conserve much of the breast. The surgeon removes the cancer, some of the breast tissue, the lining over the chest muscles below the tumor, and usually some of the lymph nodes under the arm. In most cases, radiation therapy follows.
The entire breast is removed in total mastectomy. Some lymph nodes under the arm may be removed, also.
Modified radical mastectomy refers to the procedure in which the breast, some of the lymph nodes under the arm, the lining over the chest muscles, and, sometimes, part of the chest wall muscles are removed.
Finally, the surgeon, in radical mastectomy, removes the breast, chest muscles, and all the lymph nodes under the arm. This was the standard operation for many years, but it is now typically only used when a tumor has spread to the chest muscles.
To learn more about surgery, see the Cancer Treatment module.
Radiation Therapy
A lumpectomy is followed usually by radiation therapy. During radiation therapy, high-energy x-rays are used to destroy cancer cells that may still be present in the affected breast or in nearby lymph nodes.
Radiation therapy may also be used to shrink tumors before surgery. Radiation therapy alone or in combination with chemotherapy can be used preoperatively or in lieu of surgery to destroy cancer cells and shrink tumors.
Following lumpectomy, radiation therapy to the breast and sometimes to the axilla is administered five days a week for four to six weeks. A concentrated or "boost" dose of radiation may be delivered by special implants (applicators) containing radioactive seeds, or external beam radiation.
There are times when radiation therapy is used postoperatively. This often occurs when the tumor is larger than 2 centimeters, or cancer is found in multiple lymph nodes in the axilla, or the tumor is close to the rib cage or chest wall muscles.
Intense exposure to radiation does have unavoidable side effects, including particularly fatigue, swelling, and skin changes, which gradually disappear in most cases. More serious side effects include heart and lung damage, lymphedema, and an increased risk of second malignancies.
To learn more about radiation therapy, see the Cancer Treatment module.
Chemotherapy
When a tumor is large, identified as aggressive, and/or involves the lymph nodes, some form of systemic adjuvant treatment, such as chemotherapy, is often recommended. This is usually administered postoperatively following surgery to destroy cancer cells that may have escaped into the lymph and blood vessels, thereby reducing the likelihood of a recurrence. On the other hand, a small tumor can shed cancer cells outside the breast.
Studies have shown that a combination of chemotherapy drugs is more effective than a single agent. The combination that has been favored for many years is CMF (cyclophosphamide [Cytoxan], methotrexate, and fluorouracil [5-FU]). Alternating CMF with a therapy that is Adriamycin-based, call CAF (cyclophosphamide [Cytoxan], Doxorubicin (Adriamycin), and flurorouracial [5-FU]), is becoming more common, as research demonstrate improved response rates. There are several other variations that include vincristine (Oncovin) and prednisone. Women who enter clinical trials may be offered new drugs and/or different combinations of widely used ones.
The decision of when to begin chemotherapy and how long treatment should last is very individualized and may vary from one doctor to another. Some combinations may be given in cycles lasting only two to six months; others are given for a year or more.
Investigators are looking at whether giving chemotherapy before surgery can shrink a larger tumor enough not only to permit a lumpectomy instead of a mastectomy but also to destroy cancer cells that have spread to other areas.
To learn more about chemotherapy, see the Cancer Treatment mod
Hormonal Therapy
Hormonal therapy is used to prevent the growth, spread, or recurrence of breast cancer. A pathology test on a sample of tumor tissue will reveal if the cancer has estrogen and progesterone receptors. If it has estrogen receptors, it is said to be estrogen-receptor positive; if not, it is said to be estrogen negative. The same is true of progesterone receptors.
When a tumor is said to be estrogen-positive or progesterone-positive, it means the tumor depends on the patient's natural hormones to grow.
Research has shown that if a tumor is estrogen-receptor positive, anti-estrogen therapy, such as the drug tamoxifen (Nolvadex), will block the receptor and prevent growth of cancer. Tamoxifen is used with and without chemotherapy primarily to treat women over 50. Some experts believe it is reasonable to give tamoxifen alone to low-risk, postmenopausal women and along with chemotherapy to high-risk, postmennopausal women.
Since Tamoxifen causes side effects similar to those of menopause—weight gain, hot flashes, and mood swings—younger women may choose not to take it. Most women continue on hormone therapy for two to five years, but research has not yet determined the optimal and safe duration of therapy.
There are obvious benefits to tamoxifen, but it is not without risk. Some studies have shown there may be an increased risk of endometrial cancer. Large studies are now being conducted to determine if tamoxifen will prevent cancer entirely in high-risk women. In some rare cases, removal of the ovaries is recommended, resulting in a surgically created menopause.
Clinical trials using aromatase inhibitors such as anastrozole, exemestrane and letrozole alone or in combination with Tamoxifen have shown a signification decrease in recurrence but only a small possible improvement in overall survival.
Ovarian ablation can be accomplished with surgery, radiation or hormones.
To learn more about hormonal therapy, see the Cancer Treatment module.
Immunotherapy
The immune system of the body is a natural defense against various diseases, including cancer. It also defends the body against infections and other side effects of cancer treatment. A strong immune system detects the difference between healthy cells and cancer cells, and it can get rid of those that become cancer. The immune system can be strengthened and improved by new immunotherapies. These treatments are designed to repair, stimulate, or increase the body's natural ability to fight infections and cancer.
About 25% of breast cancer patients are noted to have an overexpression of HER2/neu. A recent monoclonal antibody (immunotherapy) treatment called "herceptin" is currently used to reduce the chance of breast cancer recurrence in those patients. Bone marrow transplantation is occasionally recommended for Stage IV breast cancer patients.
As with other types of cancers, immunotherapy is also used as a treatment against breast cancer. To learn more about immunotherapy, see the Cancer Treatment module.
Systemic Therapy
Drugs Commonly Used for Treating Breast Cancer
- Combination Chemotherapy (some combinations include hormones)CMF (cytoxan, methotrexate, 5-FU)
- CMFP (cytoxan, methotrexate, 5-FU, prednisone)
- CAF (cytoxan, adriamycin, 5-FU) (also called FAC)
- CA +/- tamoxifen (cytoxan, adriamycin, tamoxifen) (also called AC +/- tamoxifen)
- CMFVP (cytoxan, methotrexate, 5-FU, vincristine, prednisone)
- PAF (L-pam/melphalan, adriamycin, 5-FU)
- L-pam and 5-FU
- Docetaxel (taxotere)
- Paclitaxel (taxol)


No comments:
Post a Comment